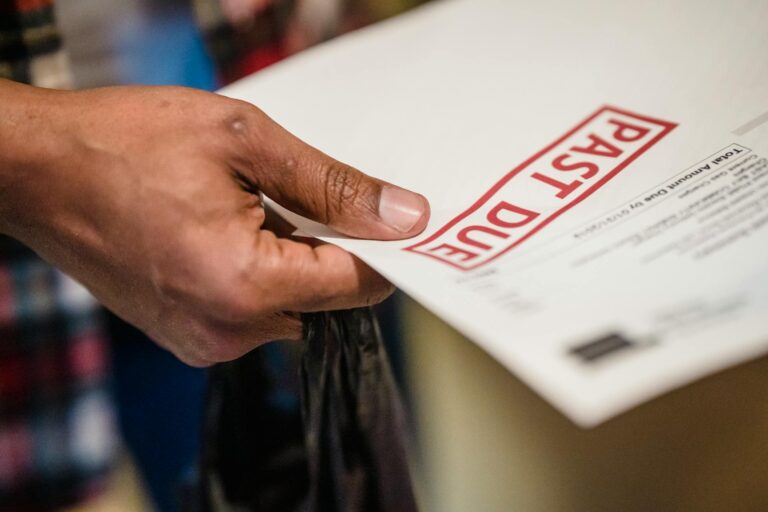
We’ve all felt it: the low-grade anxiety that follows a medical procedure. It’s not just about recovery; it’s the dread of the bill that will eventually arrive. Weeks, or even months, after you’ve left the hospital, a “surprise in the mailbox” appears—a confusing statement with an unexpected balance that causes immediate stress.
But what if that entire process was turned on its head? In response to rising patient deductibles and the growing consumerization of healthcare, a growing number of providers are shifting this difficult financial conversation to the very beginning of the patient journey. This strategy, known as pre-service collection (PSC), is a proactive approach to financial engagement. But here’s the twist: this proactive approach isn’t just about boosting the hospital’s bottom line. It’s creating a fundamentally better, less stressful, and more transparent experience for patients.
This article explores the surprising takeaways behind this shift, explaining why discussing payment upfront is becoming a cornerstone of a more satisfying healthcare experience.
A 70% Chance of Payment Becomes 30% Almost Overnight
To understand the sea change in healthcare finance, you have to start with one critical data point that reveals the core flaw of the old model. For decades, the system was reactive: provide the service first, then chase the payment later. This created a significant financial problem for providers, which is perfectly illustrated by one eye-opening statistic.
Providers have a 70% chance of collecting a patient’s payment before or at the point of service. However, once the patient has been discharged and goes home, that collection probability plummets to just 30%. This massive “40-point gap” is more than just a line on a spreadsheet. Think of a hospital’s cash flow like its blood flow; this gap creates blockages that slow the entire system down. This financial desperation is the engine behind the stressful, reactive billing system that erodes patient trust long before a collection agent ever calls. It’s the root cause of aggressive collection tactics and financial instability that ultimately impact a hospital’s ability to invest in new technology, retain staff, and maintain the very community services patients rely on.
Asking for Money Can Lead to 97% Patient Satisfaction
Here is the central paradox: how can a process focused on collecting money result in happier patients? It feels completely counter-intuitive. Yet, the data shows a direct and shocking link between a well-managed upfront financial conversation and patient happiness.
The data on this approach is shocking, with one pre-service process achieving a:
“97% patient satisfaction rating.”
This satisfaction doesn’t come from the act of paying a bill. It comes from replacing a negative, adversarial process with a supportive, partnership-based one. Instead of months of worrying about an unknown cost, patients are given a clear financial picture from the start. This proactive communication replaces the fear of a “surprise in the mailbox” with the empowerment of understanding. It proves that a collection strategy, when designed with empathy and transparency, can build trust rather than create conflict.
It’s About Predictability for You, Not Just Profit for Them
Don’t mistake this for a one-sided cash grab. A well-designed pre-service collection (PSC) system creates a more predictable and stable financial environment for everyone involved. It’s engineered to be a true “win-win.”
- For the Hospital: The benefits are clear and substantial. An effective PSC program improves cash flow by reducing the time it takes to get paid (lowering A/R days), significantly cuts losses from bad debt and write-offs, and helps them comply with increasingly strict price transparency regulations.
- For You, the Patient: The advantages are just as powerful. Through patient-friendly outreach, you receive clear cost estimates that all but eliminate billing surprises. You are offered flexible payment solutions—from digital wallets like Apple Pay and Google Pay to structured payment plans—that make managing costs less of a burden. And crucially, you gain access to financial counseling to help you navigate complex insurance benefits and explore payment assistance programs you may qualify for.
Conclusion: From Reactive Problem to Proactive Partnership
Shifting the financial conversation from a reactive, stressful event to a proactive, supportive one fundamentally changes the patient-provider relationship for the better. This approach demystifies what has long been a murky, stressful process, replacing confusion and anxiety with clarity and trust. It transforms what was once an adversarial interaction into a more predictable, respectful, and manageable part of the healthcare experience.
By addressing costs clearly and compassionately from the start, providers are not just improving their financial health; they are building a better overall experience, moving from reactive problem-solving toward a proactive partnership with their patients.
As you think about your next healthcare interaction, how might knowing that this kind of upfront financial clarity is possible change how you feel about the process?